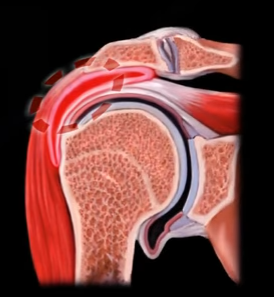
PASTA Lesions
The acronym “PASTA”, stands for: Partial- The tear has not gone all the way through the tendon; Articular surface- the inner-side of
the tendon (not the bursal side); Supraspinatus
Tendon- tear on the underside of the
rotator cuff tendon; Avulsion- usually a traumatic injury which is caused by a pulling force.
PASTA lesions are difficult to diagnose but, an arthrogram
may help in the diagnosis. The tear can be seen on an ultrasound or an MRI. The
MRI arthrogram is done in the ABER position (abduction/external rotation) and
is more accurate in showing this lesion; the arm will be above the head in the
scanner.
A normal rotator cuff is about 10-12 mm in thickness. If
exposed bone between the rotator cuff and the articular margin is more than
7mm, then there is an at least 50% thickness tear—this is a classic indication
for surgery. When the lesion is less than 50% and painful, you can debride it.
If the lesion is more than 50% and painful, you can repair it. A physician may
complete a tear to become a full thickness tear, in order to repair it.
Rotator tears can be full thickness or partial thickness
tears. The partial can be a partial articular-sided supraspinatus tendon avulsion
(PASTA) which is an articular tear—the most common type. Another type of PASTA
tear—the Bursal Tear—also referred to as a reverse pasta lesion or, it could be
a Concealed Interstitial Delamination (CID) or an inter substance tear.
PASTA tears may be associated with internal impingement,
which is different than external impingement. In the external impingement there
is a subacromial impingement (bursal pathology). In internal impingement, the
pathology is on the under surface of the cuff, so PASTA tears may be associated
with the internal impingement.