Dislocations occur more in total hip arthroplasty than in
hemiarthroplasty. Too much retroversion causes posterior dislocation. Total hip
arthroplasty is done is physiologically active elderly patients with a displaced
femoral neck fracture. Although it may increase the risk of dislocation, there
is a lower revision rate and a superior long term future outcome.
Failure of fixation
Quality and maintenance of reduction of the fracture is
important. Closed reduction can be attempted, however the reduction must be
anatomic. If it is not anatomic reduction, then open reduction should be done. Open
reduction can be done through an anterior approach or a Watson-Jones approach. When
the fixation fails, you can attempt to repeat ORIF or you may do prosthetic
replacement. It is important to note that in elderly patients, treatment of
displaced femoral neck fractures with screws may have failures and revision
rates of up to 40%.
Fracture Distal to the Fixation
This is probably due to screw placement at or below the
lesser trochanter and poor bone quality, especially if you start anteriorly and
not laterally. It is also possible that this may be due to the poor angle of
the screw fixation and multiple attempts at drilling or guide pins. Treatment
typically consists of a refixation of the femoral neck and the subtrochanteric
fracture.
Nonunion of the fracture
Femoral neck fractures are considered to be intracapsular
fractures which are at a high risk of developing a nonunion. The femoral neck
fracture is surrounded by synovial fluid and there is no extraosseous blood
supply, no periosteum, or callus formation. The fracture healing occurs by
intraosseous bone healing alone. It can present itself as groin or buttock
pain, pain with hip extension, or with weight bearing. It can occur in about 5%
of nondisplaced fractures and about 25% of displaced fractures. If it occurs in
an elderly patient, an arthroplasty must be done. If it occurs in a young
patient, a valgus intertrochanteric osteotomy. A vascularized fibular graft may
benefit the patient as well. Nonunion fractures occur more in the vertically
oriented fracture pattern with loss of reduction and varus collapse. In younger
patients, we may possibly reorient the fracture line to be more horizontal by
doing the osteotomy. Usually, the nonunion is apparent by about twelve month;
however, there may be trouble in seeing the nonunion due to the fact that there
is no periosteum and no callus in the femoral neck.
Medical Complications
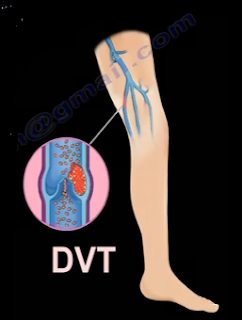
There is an increased risk of DVT of up to 80%. Some form of
prophylaxis is indicated, both mechanical and pharmacological for the patient.
It is imperative to consult the medical team for co-management. The aim of
treatment is early immobilization of the patient with pulmonary toilet. There
is a high mortality rate in the elderly—approximately 30% in one year. A surgical
delay of more than 72 hours will increase the risk of one year mortality. After
completion of the treatment, treating the osteoporosis is needed to decrease
the incidence of other fragile fractures.
Osteonecrosis (AVN)
The patient will have groin, buttock, or proximal thigh
pain. It occurs in 10% of nondisplaced fractures and in 30% of displaced
fractures. AVN could occur due to interruption of terminal branch of the medial
femoral circumflex artery by the fracture. The medial femoral circumflex artery
is the predominant blood supply to the femoral head. Usually, AVN is diagnosed
by an MRI or it can be obviously on the x-ray. Not all cases of AVN develop
evidence of radiographic collapse. AVN can be clinically significant when it is
followed by late segmental collapse.
Late segmental collapse can be seen as early as 6-9 months
following the fracture, but it is usually recognized by the second year.
Segmental collapse can be excluded if it does not occur by the third year. AVN
may occur due to an increase in the initial displacement, increase in the time
to reduction, or nonanatomic reduction. Treatment for AVN in younger patients
with less than 50% femoral head involvement may qualify for a valgus
intertrochanteric osteotomy. A free vascularized fibular graft or a total hip
replacement may be considered if the involvement of the femoral head is more
than 50%. In an elderly patient, a total hip arthroplasty will probably be
necessary.
Penetration of the screws into the hip joint.
Another possible complication is the penetration of the
screws into the hip joint. The screws should be placed within 5mm of the
articular cartilage. You can use multiple fluoroscopy images to confirm that
there is no penetration. The screws must be parallel so that it can allow the
fracture to be compressed. Make sure the threads of the screws cross the
fracture site, otherwise the threads will distract the fracture. You may use
long threads or short threads based on the situation.
Shortening
Femoral neck shortening after fracture fixation with
multiple cancellous screws can be a problem. The healed femoral neck fracture
with shortening is usually associated with a poor functional outcome.