Pain located at the heel can have several different causes.
It is important to make the correct diagnosis for the cause of the heel pain,
so that appropriate treatment can be given to the patient. Common causes of
heel pain include:
- Baxter’s Nerve Compression
- Plantar Fasciitis
- Fat Pad Atrophy
- Achilles Tendonitis
- Stress Fractures of the Calcaneus
- Lumbar Spine Radiculopathy
The sites and locations from different causes of the pain are
all very close to each other, making it difficult to determine the source of
the pain and to diagnose injuries.
In plantar fasciitis, irritation and swelling will occur at
the thick tissue on the bottom of the foot. This fascia can become inflamed and
painful, making walking more difficult. Plantar fasciitis is most severe in the
morning when patients first stand on their feet. Stretching exercises or
walking, often helps in relieving the painful tightening associated with
plantar fasciitis. Pain symptoms will intensify with prolonged exercise or
standing. Plantar fasciitis is usually
associated with a tight heel cord.
During fat pad atrophy, the fat that cushions the calcaneus
is thinned. This condition is common in elderly people and can cause
significant pain while walking. It also commonly occurs in patients with a
history of steroid injections.
Achilles Tendonitis is a chronic injury to the tendon that
joins the heel to the muscles of the lower leg, primarily occurring from
overuse. The Achilles tendon gives us the ability to rise up on our toes,
allowing for the act of walking. If a patient has Achilles tendonitis, walking
can be painful and difficult.
Stress fractures of the calcaneus can occur due to overuse
injuries. The patient will experience weight bearing pain. Stress fracture
injuries of the heel are typical in patients who engage in running sports, due
to the repetitive shock being placed on the heel. Side to side compression of
the calcaneus is painful.
Pain on the lateral side of the foot may be a result of
L5-S1 radiculopathy.
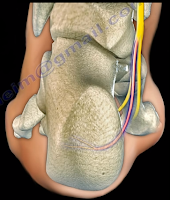
The Baxter’s nerve is the first branch of the lateral
plantar nerve. It also contributes to 20% of all heel pain causes. The Baxter’s
nerve provides motor innervation to the abductor digiti minimi muscle. When the
nerve is affected by compression, the symptoms are similar to planter
fasciitis. Entrapment of the Baxter’s nerve may cause up to 20% of heel pain,
but is still overlooked. The first branch of the lateral planter nerve is the
inferior calcaneal nerve (Baxter’s Nerve).
The nerve courses vertically between
the abductor hallucis and the quadratus plantae muscles, then makes a 90°
horizontal turn, coursing laterally beneath the calcaneus to innervate the
abductor digiti minimi muscle. The Baxter’s nerve can become entrapped within
the medial heel. The entrapment will result in heel pain, paresthesia, abnormal
sensations on the plantar aspect (bottom) of the heel, and medial heel
tenderness. There are two sites of entrapment that are typical with Baxter’s
nerve impingements. The first site is located between the fascia of the
abductor hallucis and quadratus plantae muscles. The second site is where the
nerve passes along the anterior aspect of the medial calcaneal tuberosity.
Treatment
Management is usually conservative and consists of heel
stretching exercises, rest, NSAIDs, and Orthotics. Surgery is done as a last
resort with neurolysis of the nerve after release of the deep fascia of the abductor
hallucis muscle. There is a good-excellent result in about 90% of patients
after decompression of the nerve. Involvement of the Baxter’s nerve may affect
running athletes causing pain on the medial plantar aspect of the foot.