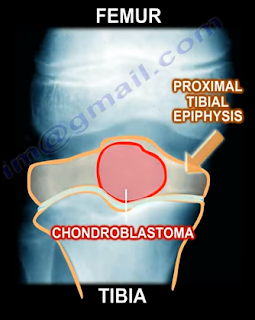
Chondroblastoma is a benign, aggressive cartilage tumor with an epiphyseal location. Chondroblastoma occurs more often in males, in younger patients between the ages of 10-25 years
of age, and in patients that may be
skeletally immature. Chondroblastoma occurs commonly at the distal femur and
the proximal tibia. 30% of chondroblastoma occur around the knee, followed by
the proximal humerus, proximal femur, and the calcaneus.
Other epiphyseal lesions include:

Other epiphyseal lesions include:
- Clear Cell Chondrosarcoma
- Occurs in older age groups
- Has a more aggressive histological pattern
- Large cells with central nuclei
- Occurs in the proximal humerus and proximal femur
- Giant Cell Tumor
- Occurs in older age groups
- Has uniform cells and the nuclei of the stroma are similar to the nuclei of the giant cells
- Osteomyelitis
- Brodie’s abscess
During the clinical examination, the patient may complain of
pain due to the tumor. The tumor abuts the joint which may cause joint symptoms
and may cross the physis. 1% of these tumor metastasize to the lung. Radiologic
images will show a lytic epiphyseal lesion with a sclerotic bony rim and sharp,
well-defined borders. There may be calcification in the matrix. An MRI will
show extensive surrounding edema.

You may find scattered giant cells and a cobblestone appearance
of the cells with chicken wire calcifications. One-third of the lesions may
have an aneurysmal bone cyst (ABC). The lesion is chondroid with polygonal
cells. The lesion will have a defined cytoplasmic border and oval shaped nuclei
with a prominent longitudinal groove (coffee bean appearance of the nuclei).
Chondroblasts can be distinguied from giant cell tumors by staining for the
S100 protein as the chondroblastoma will be reactive.
Chondroblastomas can be treated with an intralesional
curettage and bone graft. The recurrence rate is less than 10%. Some surgeons
may use adjuvants such as phenol or liquid nitrogen.