In order to remember these tests, remember that “B” comes before “O” in the alphabet and will go in this order for these procedures as well. The “B” stands for Barlow and “O” for Ortolani. When reading the word “barlow” think: “We are going out tonight!”, because the hip can be popped out of the acetabulum with this maneuver. To remember Ortolani, think: “Once we have been out, now it is time to go home!”—during the Ortolani maneuver, the femoral head is reduced back into the acetabulum.

The Ortolani Test is used to confirm the findings of the
Barlow test. The Ortolani maneuver is performed following the Barlow test to
determine if the hip is actually dislocated. The Ortolani test is performed by
the examiner flexing the hips and knees to 90 degrees. Reduction is done by
abduction of the hip and pushing the thigh anteriorly. The test is positive is
a palpable and audible clunk is heard from the hip being reduced. A hip click
is a nonspecific finding.
In summary, The Barlow Test is performed when the hip is
reduced and is used to dislocate the hip. The Ortolani Test is performed only
after the Barlow Test has been performed and the hip has been dislocated. The
Ortolani Test will reduce the hip.
Both of these tests are used for screening newborns during
the neonatal period. The hips are examined one at a time and usually the hips
are flexed during these maneuvers. Early diagnosis by these tests and
preferably with ultrasound is essential to detect hip instability and
dislocation in the neonatal period.
Treatment is directed at stabilizing the
hip that has positive Barlow and Ortolani Signs. The first born female with a
breach presentation and a positive family history are at risk of developing
developmental dysplasia of the hip (DDH). If the hip remains dislocated for weeks,
these two tests are usually not reliable. Barlow and Ortolani are not positive
after 3 months due to the soft tissue contracture around the hip region.
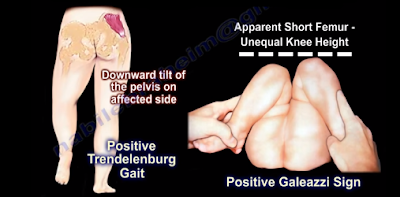
Limitation of abduction becomes the most consistent clinical findings. Children
older than 12 months will have other findings which include asymmetry of hip
abduction, a positive Trendelenburg gait and a positive Galeazzi sign.