To view my Youtube video, 'Massive Rotator Cuff Tear- Classic', click here.
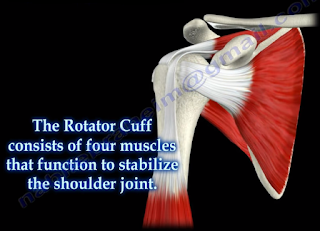
Massive rotator cuff tears are a disabling problem. These tears can cause pain, weakness, and sometimes swelling of the shoulder. The rotator cuff consists of four muscles that function to stabilize the shoulder joint: supraspinatus rotator cuff tendon, subscapularis tendon, infraspinatus rotator cuff tendon, and the teres minor rotator cuff tendon. The supraspinatus tendon is the most common of the rotator cuff tendons to become ruptured. Massive tears of the rotator cuff that are greater than 5cm usually involving both the supraspinatus and infraspinatus tendons.
 Massive tears of the rotator cuff are defined as tears
greater than 5cm, usually involving both the supraspinatus and infraspinatus
tendons. Retraction of the rotator cuff tendons along with muscle atrophy and
fatty infiltration can occur. This makes surgical reconstruction difficult with
the surgical outcome being unpredictable and less than satisfactory.
Massive tears of the rotator cuff are defined as tears
greater than 5cm, usually involving both the supraspinatus and infraspinatus
tendons. Retraction of the rotator cuff tendons along with muscle atrophy and
fatty infiltration can occur. This makes surgical reconstruction difficult with
the surgical outcome being unpredictable and less than satisfactory.
Treatment varies from physiotherapy to replacement of the
humeral head. Arthroscopic or open repair is usually the selected treatment.
Reconstruction can be done in selected cases. A rotator cuff arthropathy is
performed on massive cuff tears that are associated with superior migration of
the humeral head as well as instability and arthritis of the shoulder. The
patient will have pseudoparalysis and an x-ray will show shift of the humerus
proximally. An MRI will show massive cuff tear with retraction at the level of
the glenoid with atrophy of the muscle and fatty infiltration. A reverse shoulder
is the treatment of choice for the elderly with rotator cuff arthropathy as it
improves the pain and function. Hemiarthroplasty is the treatment for younger
patients. A standard head or a big humeral head can be selected.
A patient with a massive tear of the cuff usually develops
weakness of the shoulder and becomes unable to actively lift the arm without
assistance. Fluid collection within the shoulder may occur with a massive tear
of the rotator cuff.