Elbow Dislocation in Adults
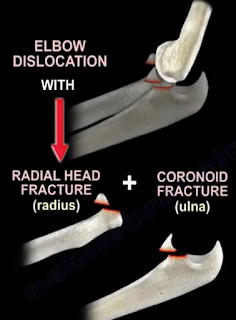
With elbow dislocations, recognize the terrible triad: elbow
dislocation, radial head fracture, and coronoid fracture. The terrible triad is
not a simple elbow dislocation; it is a complex elbow dislocation. In addition
to these three injuries of the elbow, there is always a tear of the lateral
ulnar collateral ligament. The treatment usually is reduction and splinting of
the elbow.
 This cannot be the definitive treatment; it is the initial
treatment. If no surgery is done, you will have recurrent dislocation of the
elbow. You need to do surgery for reduction and fixation of the fractures and
also to restore the elbow stability. This injury is unstable. Simple reduction
and splinting is not going to work for this injury. You have to recognize the terrible
triad which means surgery. There are multiple types of elbow dislocation based
on the position of the olecranon relative to the humerus. The most common type
of elbow dislocation is the posterolateral type. There are two basic types of
elbow dislocations: simple and complex. Simple elbow dislocations have no
fracture seen, and are usually a ligamentous injury. Complex elbow dislocations
have associated fractures in addition to the ligamentous injury. With any elbow
dislocation, you need to check the shoulder and the wrist for injuries and
fractures because it can occur in up to 15%. When you have a simple dislocation
of the elbow, you need to reduce it and then check the range of stability of
the elbow. If you find that the elbow is stable with range of motion, then you
will do a short period of immobilization with a posterior splint for
approximately one week with the elbow in about 90 degrees of flexion. Then start
active range of motion of the elbow. Recurrence of the dislocation is rare
(less than 1%). If you keep the elbow immobilized more than 3 weeks, there will
be severe stiffness of the elbow. Surgery should be done if the dislocation is
irreducible, if there is associated fracture, or if you are unable to maintain
stability of the elbow. After immobilization and early range of motion of the
elbow, you will see the patient and do follow up x-rays to check joint
congruity and to make sure that the elbow reduction is maintained. To treat the
terrible triad, you should initially do a closed reduction. Open reduction and
internal fixation of the coronoid (if possible), of the radial head or excise
the radial head with radial head arthroplasty if the radial head is
unreconstructable. In addition, you will do lateral ulnar collateral ligament (LUCL)
repair. Never excise the radial head alone in this situation. For an elbow
dislocation with olecranon fracture, do open reduction and plate fixation.
K-wires and tension band is not strong enough to hold the fracture and
stabilize the elbow at the same time. For an elbow dislocation with a radial
head fracture, do fixation or replacement of the radial head (never do excision
of the radial head alone in this situation). The LUCL is the most important
lesion in recurrence or persistence of instability of the elbow following
simple elbow dislocation.
This cannot be the definitive treatment; it is the initial
treatment. If no surgery is done, you will have recurrent dislocation of the
elbow. You need to do surgery for reduction and fixation of the fractures and
also to restore the elbow stability. This injury is unstable. Simple reduction
and splinting is not going to work for this injury. You have to recognize the terrible
triad which means surgery. There are multiple types of elbow dislocation based
on the position of the olecranon relative to the humerus. The most common type
of elbow dislocation is the posterolateral type. There are two basic types of
elbow dislocations: simple and complex. Simple elbow dislocations have no
fracture seen, and are usually a ligamentous injury. Complex elbow dislocations
have associated fractures in addition to the ligamentous injury. With any elbow
dislocation, you need to check the shoulder and the wrist for injuries and
fractures because it can occur in up to 15%. When you have a simple dislocation
of the elbow, you need to reduce it and then check the range of stability of
the elbow. If you find that the elbow is stable with range of motion, then you
will do a short period of immobilization with a posterior splint for
approximately one week with the elbow in about 90 degrees of flexion. Then start
active range of motion of the elbow. Recurrence of the dislocation is rare
(less than 1%). If you keep the elbow immobilized more than 3 weeks, there will
be severe stiffness of the elbow. Surgery should be done if the dislocation is
irreducible, if there is associated fracture, or if you are unable to maintain
stability of the elbow. After immobilization and early range of motion of the
elbow, you will see the patient and do follow up x-rays to check joint
congruity and to make sure that the elbow reduction is maintained. To treat the
terrible triad, you should initially do a closed reduction. Open reduction and
internal fixation of the coronoid (if possible), of the radial head or excise
the radial head with radial head arthroplasty if the radial head is
unreconstructable. In addition, you will do lateral ulnar collateral ligament (LUCL)
repair. Never excise the radial head alone in this situation. For an elbow
dislocation with olecranon fracture, do open reduction and plate fixation.
K-wires and tension band is not strong enough to hold the fracture and
stabilize the elbow at the same time. For an elbow dislocation with a radial
head fracture, do fixation or replacement of the radial head (never do excision
of the radial head alone in this situation). The LUCL is the most important
lesion in recurrence or persistence of instability of the elbow following
simple elbow dislocation. The injury progresses from lateral to medial. The lateral collateral ligament fails first, and it avulses proximally at the lateral epicondyle. The medial collateral ligament (MCL) fails last. In varus posteromedial rotary instability, there is an elbow injury plus LUCL tear, plus coronoid fracture which involves the medial facet of the coronoid. Treatment for chronic dislocation is open reduction capsular releases with hinge external fixation and early range of motion. Loss of terminal extension is a complication of elbow dislocation. Usually for decreased range of motion of the elbow, you will do static progressive splinting between 6-10 weeks. No manipulation of the elbow is done, which is different from the knee after total knee replacement, where you can do manipulation up to three months. With heterotopic ossification, do excision. Remove the myositis and excise the posterior part of the MCL to allow more flexion. To be functional, the range of motion of the elbow should be between 30-130 degrees. Some physicians suggest that if the flexion is less than 100, you will do release of the posterior bundle of the MCL in addition to release of the ulnar nerve. If you want more flexion of the elbow, excise the posterior part of the MCL.









