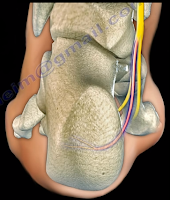
A SLAP tear is a tear that occurs where the biceps tendon
inserts into the superior labrum. A SLAP tear is different from a Bankart
lesion. SLAP tears are not common and can be hard to diagnose. Symptoms of a
SLAP tear include: pain deep within the shoulder or in the back of the
shoulder, as well as catching, popping, or clicking sensations. The patient may
also experience pain when throwing a ball with a decrease in velocity and the
feeling of having a dead arm after pitching. Patients will also experience pain
with overhead activity which mimics impingement syndrome. This typically
affects throwing athletes. When the biceps tendon is involved, pain may also be
located at the front of the shoulder. A SLAP tear can be an isolated lesion or
it can be associated with internal impingement, articular sided cuff tear, or
instability.
A SLAP tear is diagnosed with a clinical examination and
testing. The O’Brien’s test is the most commonly used test. Multiple tests are
usually used including the anterior slide test and the clunk test. An MRI with
contrast is the best imaging technique. When performing the O’Brien’s test, the
patient is standing or sitting with the arm at 90° of flexion, 10° of
adduction, and full internal rotation with the forearm pronated. The examiner applies pressure to the forearm
and instructs the patient to resist the applied downward force. Pain at the
shoulder joint suggests a SLAP lesion. Decrease in pain of the shoulder joint
on supination of the arm is suggestive of a SLAP tear.
Treatment consists of physical therapy, anti-inflammatory
medications, injections, and surgery (when conservative treatment fails). If
surgery is necessary, a labral debridement will be performed for minor tearing
and fraying. Biceps Tenodesis is becoming popular, as it is a procedure that
cuts the biceps tendon where it attaches to the labrum and reinserts it in
another area, usually in front of the shoulder. A biceps tenotomy is a
procedure that cuts the biceps tendon from the glenoid, releasing the long head
of the biceps tendon from its attachment allowing it to fall into the upper arm
out of the shoulder joint. A biceps tenotomy is probably best suitable for some
elderly patients. A SLAP repair is a procedure which uses sutures to anchor the
torn labrum to the glenoid. This repair is usually done for athletes and
patients under the age of 40 years.