In general, doctors treat patients for pain due to injury or
surgery. Pain intensity varies from person to person and it can be related to
stress, distress, coping strategies, and physiological factors. The physician
should work with the patient for better pain control and for safer prescribing
of medications. The best pain relief is
self-efficacy and resilience. We have found that giving the patient a teddy
bear helps to relieve their pain and anxiety, giving the patient comfort and
confidence in the system.
Showing posts with label pain. Show all posts
Showing posts with label pain. Show all posts
Thursday, November 7, 2019
Wednesday, September 26, 2018
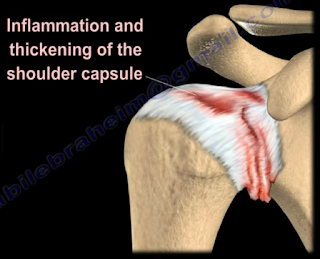
Adhesive Capsulitis, Frozen Shoulder
Adhesive Capsulitis, or frozen shoulder, is a painful progressive
loss of shoulder motion. It affects both active and passive movement of the
shoulder joint. The shoulder will be stiff and painful and occurs due to
inflammation, fibrosis, scarring, and contraction of the capsule. A normal
shoulder joint capsule is elastic and allows great range of motion.
Inflammation and thickening of the shoulder capsule and may lead to adhesive
capsulitis. Frozen shoulder may occur without any specific cause, however it
may be triggered by a mild trauma to the shoulder.
This condition develops slowly and goes through three
phases:
- Pain and freezing
- Stiffness or frozen
- Resolution
During the pain and freezing phase, the pain is worse at
night and increases with any movement. This phase will last several months.
During the second phase, range of motion is limited as pain is diminishing.
This may last up to one year. The resolution phase may begin overtime and may
last up to three years.
Conditions associated with frozen shoulder include:
- Diabetes
- Thyroid problems
- Auto immune disease
- Stroke
- Rheumatoid arthritis
- Trauma or post-surgery
A patient with frozen shoulder will have loss of both active
(movement without assistance) and passive (movement with assistance) motion.
External rotation of the shoulder is very limited and the condition is
self-limiting and may resolve on its own. X-rays are needed to rule out
degenerative arthritis. An MRI or
arthrogram will show small fluid in joint cavity. Rotator cuff may be normal
and synovitis and narrowing of the rotator cuff interval is usually seen.
Treatment consists of anti-inflammatory medications,
physical therapy, injections, and manipulation under anesthesia. Surgery will
be done in the form of a release of the capsule when nonoperative methods fail.
The physician should always check the patient for diabetes.
Labels:
Arm injuries,
arm pain,
Dr. Nabil Ebraheim,
education,
injury,
Medical Education,
Medical School,
medicine,
MRI,
Nabil Ebraheim,
Orthopaedic Surgery,
Orthopaedics,
Orthopedics,
pain,
Shoulder,
shoulder pain
Tuesday, August 14, 2018
Triplane Fracture of the Distal Tibia
A triplane fracture of the distal tibia usually occurs
during adolescence and occurs before complete closure of the distal tibial
physis. The distal tibial physis (growth plate) is a weak area which closes
from central to medial, with the lateral side being the last part to close. A
Triplane fracture is a Salter-Harris Type IV Fracture, involving all three
planes, the coronal (metaphysis), transverse (growth plate), and sagittal (epiphysis).
The fracture has several variations and occurs due to external rotation forces.
This fracture typically occurs in patients between 12-15 years of age.
Triplane fractures are complicated three-dimensional
fractures. A two-part fracture is a Salter-Harris Type IV. A Three-part
fracture is a combination of Salter-Harris Type III in an AP view and a Type II
in a lateral view. CT scans are helpful.
An ORIF is necessary if there is displacement of the
fragments of more than 2 mm.
Tuesday, July 17, 2018
Intra-articular Extensile Approach for Tibial Plateau Fractures
 Several types of tibial plateau fractures are a complex
management problem. The knee joint may have a significant comminution and
depression, and the physician may need to take an extensile approach for
reduction and fixation of this fracture. Personally, I use the intra-articular
extensile approach for tibial plateau fracture reduction and fixation. In
general, fracture of the tibial plateau is a complicated problem.
Several types of tibial plateau fractures are a complex
management problem. The knee joint may have a significant comminution and
depression, and the physician may need to take an extensile approach for
reduction and fixation of this fracture. Personally, I use the intra-articular
extensile approach for tibial plateau fracture reduction and fixation. In
general, fracture of the tibial plateau is a complicated problem.
A vascular evaluation is necessary. The ankle-brachial index
(ABI) is needed in some types, such as in medial plateau fractures or in severe
types, such as Schatzker Type V or Type VI. The ABI should be more than 0.9.
Usually, medial tibial plateau fractures are considered to be a knee
dislocation. A fasciotomy may be needed if compartment syndrome occurs. The soft
tissue condition may be bad, and an external fixator may be initially used
until the soft tissue condition improves.
The association between tibial plateau fractures and meniscal
tear is not uncommon. A lateral plateau fracture will create a lateral meniscal
tear, while the medial plateau fracture will cause a medial meniscal tear. A
tear of the meniscus is usually peripheral. It should be recognized and dealt
with. The physician may want to look at the x-ray and see if there is a
depression or separation of more than 6mm, as this indicates a high chance of
meniscal tear.
Tuesday, June 19, 2018
Isolated Fibular Fractures
Fibular fractures are usually associated with a complex
injury, however they can be an isolated fracture. Complex injuries where a
fibula fracture can occur include: fracture of the fibula and tibia, ankle
fracture, pilon fracture, and Maisonneuve fractures.
Maisonneuve fractures
involve a fracture of the proximal fibula associated with an occult injury of
the ankle. Isolated fibular fractures are rare and usually the result of direct
trauma. The fibula carries about 15% of the axial load and is the site of
muscle attachment for the peroneus muscles and the flexor hallucis longus
muscle. Check the patient who has a fibular fracture and no other fracture
involving the tibia to rule out a possible Maisonneuve fracture, especially if
there is no history of direct trauma to the leg. A high index of suspicion is
necessary to diagnose and treat this injury. For high fibular fractures, the
physician should look for signs of syndesmotic injury. Syndesmotic injury may
include an unexplained increase in the medial clear space or the tibiofibular
clear space is widened (should be less than 5mm). The x-ray will show the
fracture to be rotational or oblique. Maisonneuve fractures require surgery to
fix the syndesmosis.
Treatment will consist of reduction and fixation. It is
important to determine if the injury is a Maisonneuve fracture or an isolated
fibular fracture. An isolated fibular fracture will not need surgery.
Labels:
bones,
Causes and Symptoms,
causes and treatment,
Dr. Nabil Ebraheim,
education,
Fractures,
Nabil Ebraheim,
Orthopaedic Surgery,
Orthopaedics,
Orthopedics,
pain,
reduction,
screws,
trauma,
treatment
Tuesday, April 3, 2018
Cauda Equina—Central Disc Herniation
Disc herniations usually occurs posterolaterally, but it may
also be central. The cauda equina is composed of several nerves within the
lower end of the spinal canal. The top of the spinal cord is a tubular bundle
of nervous tissue extending from the brain.
The following section of the spinal
cord is called the Conus Medullaris and is the lower end of the spinal cord.
The Cauda Equina is made up of multiple nerve roots beginning at the level of
L1.
The most common disc herniation is the Posterolateral Disc
Herniation. This type of herniation is a nerve root injury, which will cause
changes to both the sensory and motor skills as well as the reflexes. A
posterolateral disc herniation usually affects the foot and ankle, and may
cause unilateral leg pain and weakness. Observe for a positive straight leg
raising test. These herniations are usually initially treated with conservative
methods.
A central disc herniation will cause cauda equina syndrome,
which is a compression over the lumbosacral nerve roots. This compression will
cause more back pain than leg pain, and bladder and bowel symptoms will be
evident. This herniation is considered a surgical emergency.
Wednesday, March 21, 2018
Malunions of the Clavicle
It is difficult to reduce and maintain the reduction of
clavicle fractures as there will be deforming forces in the midshaft area of
the clavicle. The clavicle will heal regardless as to if a sling or figure 8
strap is used. Despite the presence of a bump, fracture displacement, and
deformity, healing of the fracture still occurs rapidly. Healing occurs in
about 85% of cases, however, the clavicle will not look aligned due to the
difficulty in reducing the fracture. It is hard to achieve a reduction of these
fracture without surgery. Without surgical reduction, the fracture may end with
some degree of malunion and possible shortening of the clavicle. The fragments
will not line up with the distal fragment appearing to be downward and
anteriorly rotated. Shortening is clinically significant because it alters the
dynamics of the muscles around the shoulder. It also narrows the
costoclavicular space. The patient may complain of decreased shoulder strength
and endurance if the patient had a displaced midshaft clavicle fracture that
healed with more than 2 cm of shortening.
What are the symptoms of clavicle malunion?
Pain, easy fatigability, cosmetic problems (especially in
females), neurological dysfunction (possible involvement of the brachial plexus—especially
the ulnar nerve), and the patient may have thoracic outlet syndrome.
 X-rays should be done of both shoulders. Bilateral panoramic
views are beneficial in order to measure the shortening. The physician will
also want to check the amount of overlap at the ends of the clavicle.
X-rays should be done of both shoulders. Bilateral panoramic
views are beneficial in order to measure the shortening. The physician will
also want to check the amount of overlap at the ends of the clavicle. Treatment
Surgical treatment of the malunion may be successful in
restoring the function and relieving the pain. A clavicle osteotomy is done in
the plane of the healed fracture. The fracture is recreated with correction of
the deformity and the length of the clavicle is restored. A local or iliac
crest bone graft can be used if needed.
If an osteotomy is done with reduction of the clavicle to
its preinjury position and leaves a significant bone defect, the physician will
need a tricortical piece of bone at the osteotomy area. It is probably better
to use a precontoured clavicle plate in the superior position with six
cortices, three placed on each side of the osteotomy.

Wednesday, March 14, 2018
Elbow Joint Dislocations
An Elbow dislocation occurs when the radius and ulna bones
of the forearm move out of place from the humerus bone of the upper arm. There
are two basic types of elbow dislocations:
Simple
No fracture of the bones around the elbow joint
Usually ligamentous injury
Complex
Fracture has occurred along with ligamentous injury
Simple elbow dislocations typically occur when the patient
falls onto an outstretched hand. Injury progression from lateral to medial in
most patients. Posterolateral simple dislocations are the most common, occurring
approximately 90% of the time.
The proximal ulna and radius are displaced
posterolaterally relative to the distal humerus. Postemedial dislocations occur
at the proximal ulna and radius and are displaced posteromedially relative to
the distal humerus. In medial dislocations, the proximal ulna and radius are
displaced medially relative to the distal humerus. With lateral dislocations,
the proximal ulna and radius are displaced laterally relative to the distal
humerus. Anterior dislocations are rare, as they result from a direct force
applied to the posterior aspect of the forearm with the elbow in a flexed
position. Anterior dislocations occur when the proximal ulna and radius are
displaced anteriorly relative to the distal humerus. If stable, simple acute
fractures can be treated with a closed reduction and a splint for two to three
days (no more than two weeks) in addition to range-of-motion exercises and
physical therapy. Unstable simple fractures are rare, but can be stabilized by
ligament repair and/or by the use of an external fixator or cross pinning of
the joint in the elderly.
Chronic Elbow dislocations will need to be treated with an
open reduction and external fixator and is usually hinged. Recurrent elbow
dislocations (diagnosed by pivot shift) occurs due to a deficiency of the
lateral collateral ligament and is treated by a reconstruction of the
ulnohumeral ligament with a tendon graft.
Friday, March 2, 2018
Clay Shoveler’s Fracture
A clay shoveler’s fracture is a stable fracture through the
spinous process of the vertebra C6-T1 and typically occurs at the level of C6
or C7. Clay shoveler’s fracture gets its name from the common injury suffered
by men diffing deep ditches in Australia during the 1930s.
Powerful
hyperflexion of the neck combined with contraction of the paraspinous muscles
during shoveling is the typical mechanism of injury. The tremendous force pulls
on the spinous process, producing an avulsion fracture.
The fracture is best seen on a lateral view x-ray. There
will be a ghost sign on AP view x-rays—double spinal process of C6 or C7,
resulting from a displaced fractured spinous process.
Stable fractures can be treated nonoperatively, utilizing a
collar and physical therapy.
Tuesday, February 13, 2018
Pronator Teres Syndrome
The nerve that is involved in pronator teres syndrome is the
median nerve. Pronator Teres Syndrome is caused by a compression of the median
nerve at the level of the elbow which occurs more in women. In the forearm, the
median nerve runs between the two heads of the pronator teres muscle and then
it lies between the flexor digitorum superficialis and flexor digitorum
profundus muscles. This syndrome may be associated with medial epicondylitis.
The principle symptoms of numbness in the radial 3 ½ fingers as well as thenar
weakness which may be mistakenly attributed to carpal tunnel syndrome.
 The most common cause of entrapment is due to compression of
the median nerve between the two heads of the pronator teres muscle. This
commonly occurs in people who perform repetitive forceful pronation of the
forearm. Compression may be due to the thickening of the bicipital aponeurosis.
The aponeurosis crosses from lateral to medial over the antecubital fossa and
may irritate the median nerve. Compression of the nerve may also occur due to
the fibrous arch of the origin of the flexor digitorum superficialis (FDS).
The most common cause of entrapment is due to compression of
the median nerve between the two heads of the pronator teres muscle. This
commonly occurs in people who perform repetitive forceful pronation of the
forearm. Compression may be due to the thickening of the bicipital aponeurosis.
The aponeurosis crosses from lateral to medial over the antecubital fossa and
may irritate the median nerve. Compression of the nerve may also occur due to
the fibrous arch of the origin of the flexor digitorum superficialis (FDS).
The median nerve runs down the medial side of the arm and
passes 2 ½ to 4 cm below the level of the medial epicondyle before it enters
between the two heads of the pronator teres. About 1% of
patients have a medial
supracondylar humeral spur about 5cm proximally to the medial epicondyle. The
ligament of Struthers is attached to this bony projection which connects the
process to the medial epicondyle. The bony process points towards the elbow
joint and the median nerve can become compressed by the supracondylar spur. The
median nerve can also become trapped by the ligament of Struthers that extends
from the supracondylar process to the medial epicondyle. The ligament of
Struthers is different from the arcade of Struthers, which deals with the
compression of the ulnar nerve around the elbow.
 Paresthesia in these lateral 3 ½ fingers may occur with the compression
of the median nerve at the elbow region or at the carpal tunnel region. These symptoms are similar to carpal tunnel syndrome but the symptoms are worse with
rotation of the forearm. The patient will complain of dull aching pain over the
proximal forearm with no nighttime symptoms. The pain is usually worsened by
repetitive or forceful pronation. Tenderness of palpation to the pronator teres
muscle will be detected. The median nerve gives off a palmar cutaneous branch
before entering the carpal tunnel. Sensory disturbances over the palm of the
hand occur due to involvement of the palmar cutaneous branch of the medial
nerve and this occurs proximal to the carpal tunnel. Sensory disturbances in
this area indicates median nerve problems proximal to the carpal tunnel. This differentiates
between carpal tunnel syndrome and pronator teres syndrome.
Paresthesia in these lateral 3 ½ fingers may occur with the compression
of the median nerve at the elbow region or at the carpal tunnel region. These symptoms are similar to carpal tunnel syndrome but the symptoms are worse with
rotation of the forearm. The patient will complain of dull aching pain over the
proximal forearm with no nighttime symptoms. The pain is usually worsened by
repetitive or forceful pronation. Tenderness of palpation to the pronator teres
muscle will be detected. The median nerve gives off a palmar cutaneous branch
before entering the carpal tunnel. Sensory disturbances over the palm of the
hand occur due to involvement of the palmar cutaneous branch of the medial
nerve and this occurs proximal to the carpal tunnel. Sensory disturbances in
this area indicates median nerve problems proximal to the carpal tunnel. This differentiates
between carpal tunnel syndrome and pronator teres syndrome.
There are specific provocative tests that produce the pain
and distal paresthesia that are used to localize the site of compression. The
Tinel’s sign at the wrist and the Phalen’s test will be negative. The Median
nerve compression tests are negative at the carpal tunnel; however, there will
be a positive Tinel’s sign at the proximal forearm. There will be abnormal
sensation in the “palmar triangle”. When compression of the nerve involves the
supracondylar process, the test is considered positive if symptoms of tingling
worsen while tapping on the spur.
Occassionally, the spur can be felt. The
pronator teres muscle can be assessed as the cause of the median nerve
compression in different ways. Resisted forearm pronation with elbow flexion
will test for compression at the two heads of the pronator teres muscle. During
this test, the patient’s forearm is held in resisted pronation and flexion.
While remaining in a pronated position, the forearm is gradually extended.
Compression of the median nerve may also be tested by: resisted elbow flexion
with forearm supination (compression at the bicipital aponeurosis) and resisted
contraction of the FDS to the middle finger (compression at the FDS arch).
Differential Diagnosis
C6/C7 Radiculopathy occurs due to involvement of the nerves
at these levels which will cause numbness of the thumb, index, and long
fingers, as well as weakness of the muscles of the forearm that are innervated
by the median nerve. The radial nerve part of C6-C7 will show normal function
of the wrist extensors and the triceps.
X-rays, imaging and nerve conduction studies may be helpful
in the diagnosis.
Treatment typically consists of rest, splints, and NSAIDs.
Surgical decompression of the median nerve through all 4 or 5 possible sites of
compression when non-operative management fails for 3-6 months. The results of
surgery are variable. Full recovery is not always seen in all patients as only
about 80% of patients improve from surgery. The skin incision may leave an
unsatisfactory scar.
Friday, January 12, 2018
PIP Dorsal Fracture Dislocation
Proximal interphalangeal (PIP) dorsal fracture dislocations
can be challenging in management. In PIP dorsal fracture dislocations, there
is an involvement of the articular surfaces of the joint. These injuries are the
most disabling PIP joint injuries. A reduction of the middle phalanx on the
condyles of the proximal phalanx is the primary goal of treatment. The patient
frequently presents with a chronic dorsal subluxation due to delay in seeking
treatment or from failed treatment.
85% of motion for grasping objects occurs at the PIP joint.
The PIP joint has the largest arc of motion (120 degrees) of the three joints
in each digit.
There are three different types of injury:
- Hyperextension
- Impact Shear
- Pylon
In cases of Hyperextension injuries, the size of the
fragment can range from a small piece of bone, up to 30% of the joint surface
with minimal comminution (usually stable).
In order to provide accurate treatment, the physician will want to test
the stability of the fracture and apply a dorsal blocking splint. It is
important to observe the lateral view for any subluxation.
Impaction/Shear injuries are produced by an axial load
applied to a slightly extended or flexed PIP joint. The middle phalanx is
driven over the head of the proximal phalanx with comminution and impaction of
the base of the middle phalanx. These injuries are characterized by the loss of
the volar plate tether. A 50% loss of the palmar of the middle phalanx base
will make the PIP joint unstable. The extensor tendon and superficialis tendon
will aggravate the dorsal subluxation. Splints will be inadequate if the injury
is not stable. Treatment will include skeletal traction and early range of
motion. An open reduction and internal fixation may be necessary if the
fragment is large enough. A Palmar Plate Arthroplasty may be considered to
advance the palmar plate into the defect. This procedure will support the
palmar plate by filling the defect behind it with fracture chips, bone graft,
or by a superficialis slip. Chronic impaction/shear cases are a difficult
problem and can be treated with an arthrodesis or volar plate arthroplasty.
A pylon fracture results from an axial force that fractures
the volar and dorsal articular surfaces with impaction on the central part. A
pylon fracture is not a true fracture dislocation and will not have a good
outcome. Dynamic external traction should be done in order to help in
ligamentotaxis. Early range of motion is important for remodeling of the joint.
Classification of a PIP Dorsal Fracture Dislocation will
depend on the degree of involvement of the articular surface.
- Type I (stable) <30%
- Type II (tenuous)= 30-50%
- Type III (unstable) > 50%
Treatment will consist of a Dorsal Extension Blocking Splint
if the PIP can be reduced in less than 30% of flexion. If less than 40%, the
joint involved and stable. For Type I and Type II fractures, decrease the
flexion gradually every week. Type III fractures will require ORIF, volar plate
arthroplasty, or hemi-hamate graft (if >40% joint involved and unstable).
With a Hemi-Hamate Graft, the damaged palmar lip of the
middle phalanx with a size matched portion of the hamate bone obtained from its
distal dorsal articular surface between the 4th and 5th
metacarpals. It restores both articular congruity and osseous stability.
Extension block pinning is probably a helpful technique. Treatment must provide
stable reduction to allow for early mobilization.
Recognizing Subluxation
AP and lateral x-rays are necessary for diagnosis. An AP
view will help to recognize impaction fractures. Subluxation can be missed on x-rays. The
physician will want to look for the characteristic “V” sign of diverging joint
surfaces, which indicates injury and subluxation.
If a reduction of the avulsion fracture is achieved with
less than a 30 degree bend, nonoperative treatment is a good choice. However,
if it takes more than 30 degrees of flexion to reduce the fragment, this may be
an indication for surgery.
Subscribe to:
Posts (Atom)