Frozen Shoulder Adhesive Capsulitis - Everything You
Need To Know
https://www.youtube.com/watch?v=VhfaPe8f7g0
Frozen shoulder (adhesive
capsulitis)
The frozen shoulder can be
associated with diabetes or thyroid disease.
It may be the initial presenting symptom for these conditions. The exact details of this relationship remain
poorly understood. Ever patient with a
frozen shoulder should have the HbA1c and TSH levels tested. Also, check for arthritis, rheumatoid factors
and antinuclear antibodies. Most
patients with frozen shoulder are female between the ages of 40 and 60 years
old. And frozen shoulder, the patient
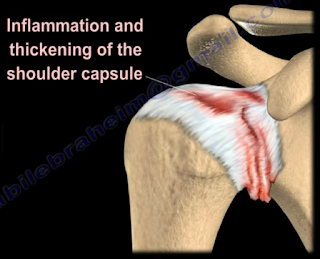
will lose both the active and the passive range of motion of the shoulder. The patient develops pain, which means that
there is inflammation with early fibrosis of the joint capsule, leading to
joint stiffness. The active and passive
global motion, especially external rotation, will be reduced compared to the
other side. The shoulder pain and motion
loss is usually not related to trauma.
It is an idiopathic process that results in shoulder pain and loss of motion
due to contracture of the capsule. The
essential lesion involves the coracohumeral ligament and the rotator
interval. The synovial inflammation and
capsular fibrosis results in pain and joint volume loss. Check for previous trauma or fractures. Rule out shoulder joint arthritis and rule
out posterior dislocation of the shoulder.
It can also occur post-surgery from a rotator cuff tear. It may also be associated with dupuytren
disease and cervical disc disease. Check
for medical comorbidities such as stroke or cardiac diseases. The x-ray will exclude trauma, malignancy, arthritis,
calcific tendinitis, impingement, and AC joint arthritis. And frozen shoulder, the humeral head will
remain in its normal location.
MRI
There is a space reduction in
the axillary recess. Rotator cuff
strength is normal by exam and on the MRI.
The pain and stiffness lasts beyond 6 months, then you can do
manipulation of the shoulder under anesthesia.
There is a 50% failure rate in diabetics. The diabetes is associated with a much worse
prognosis and poor outcome for surgical and nonsurgical treatment.
Treatment
·
Nonoperative
o
This should be
done for at least 3 to 6 months.
o
Supervised or
home-based capsular stretching program +/-intra-articular steroid joint
injection.
o
Nonsteroidal
anti-inflammatory medication
·
Surgery
o
Capsular release
(arthroscopic or open) and release the intra-articular and subacromial
adhesions.
o
The axillary
nerve may be injured during release of the capsule.
o
Utilize surgery
in patients that have failure of initial conservative treatment for 3 months,
and the patient remains functionally limited.